Pituitary Gland Disease, Symptoms, Diagnosis And Treatment
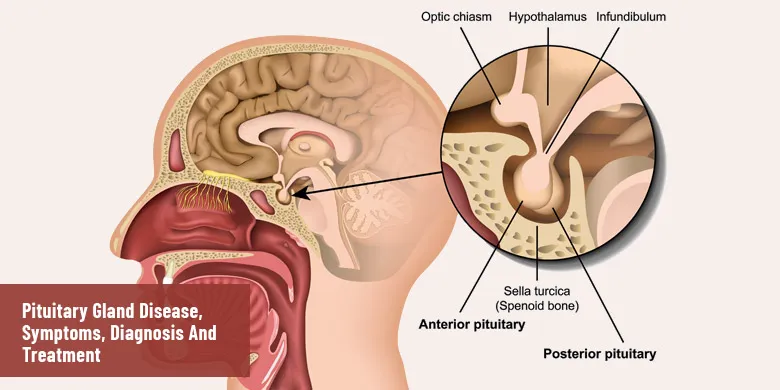
Attached to the base of the brain, this pea-sized endocrine gland does the marvelous job of producing several hormonal secretions that control various organs and regulate a number of vital functions, including the maintenance of homeostasis, growth, birth and reproduction, and so on. It won’t be illogical to claim that any disturbance or abnormality in the structure and functioning of the pituitary gland can have serious consequences for one’s health and life. There have been discovered many different types of pituitary gland disorders. Some are mild while others are severe and can even be life-threatening. However, proper diagnosis and timely treatment can save you from any severe consequences and complications. Let’s have a look at the list of pituitary gland disorders, while learning about the symptoms, diagnosis and treatment of each.
Tumors of The Pituitary Gland
Most of the tumors of the pituitary are benign and do not travel to and affect adjacent brain tissues. The tumors can be of two major types, that is, either hormone secreting or non-secreting. It means, sometimes, even after the development of tumor, this gland is able to produce right quantity of hormone secretion. However, as the tumor grows in size, the adjacent tissues of brain get compressed.
Symptoms:
- Presence of extra hormones in the blood.
- Headache and loss of vision.
- Weakness of muscles and bones.
- High blood pressure and flushing of the face.
- Irregularity in the heartbeat.
- Enlargement of hands or feet (acromegaly)
- Lower sex drive and impotence.
- Loss of body hair and weight gain.
- Nausea, vomiting and dizziness.
Diagnosis:
Your healthcare provider may suggest urine and blood tests for determining the hormone levels in the body. For detecting the presence of tumor in the pituitary, the scanning techniques, like MRI and CT can prove to be very helpful. However, making difference between a cancerous and noncancerous tumor is fairly difficult. A cancerous tumor would be confirmed if it spreads from pituitary to any other part of the body, such as brain, spinal cord, nearby bone and meninges. A noncancerous tumor, on the other, has less chances of spreading to and affecting other part of the body.
Treatment:
The choice of treatment method for a pituitary gland tumor depends upon the nature (cancerous or noncancerous), size (small or large) and level of severity (whether it has spread to other parts). Different therapeutic measures that are in vogue include drug therapy, use of radiation and surgery.
Acromegaly
Acromegaly is characterized by the over-production of the GH (Growth Hormone) after an individual reaches puberty. The malady is owed to a number of factors, like the growth of a tumor known as pituitary adenoma. The symptoms cannot be noticed for years, ultimately leading to the severity of disfigurement, and if treatment is delayed, the victim may suffer from premature death. The treatment of acromegaly is carried out through various means including drug administration, surgery or radiation therapy.
Symptoms:
- Enlargement of bones and muscular tissues in the arms, face and hands.
- A prominent brow and enlargement of tongue or jaw.
- Swelling and pain in the joints that may limit movement.
- Weight gain and excessive hair growth in women.
- Headache, fatigue and muscle weakness.
- Enlargement of the sebaceous (oil producing) glands in the skin.
- Profuse sweating and inability to sleep.
Diagnosis:
Blood tests can be used to determine excess amount of growth hormone (GH). If this be the case, there is possibility of acromegaly. This may sometimes be misleading. So, the doctors may apply glucose tolerance test. Meanwhile, the imaging studies like X-Rays, MRI and CT scan can be very helpful in finding out the location and size of the pituitary tumor.
Treatment:
The choice of the type of treatment of acromegaly is based on the age and overall health of the victim. Here the primary purpose is to bring growth hormone production levels back to the normal and maintain normal pituitary functions. Doctors regard surgery as the first option to treat the condition of acromegaly. Alternative treatment measures include radiation and medication.
Growth Hormone Deficiency
Decreased synthesis of growth hormone in children results in dwarfism. The condition expresses itself through delayed growth and shortness of body stature. Muscular weakness, decreased bone mass, fatigue and obesity are some of the common symptoms among the victims. The treatment is possible both in childhood and adulthood that is carried out by the replacement of GH with rHGH which is a recombinant type of human growth hormone. This alternative form of chemical messenger is produced by some bacteria which are genetically engineered.
Symptoms:
- Short body height, younger looks and round faces.
- Reduced bone strength leading to frequent fractures, especially in older adults.
- Feeling of tiredness and lack of stamina.
- Depression and lack of concentration.
- Poor memory.
- Emotional distress and bouts of anxiety.
Diagnosis:
If a child is not meeting the milestones of weight and height, they must be diagnosed for the growth hormone deficiency. As usual, blood test will be helpful in measuring the level of growth hormone in the body. The level of bone growth in a child’s hand can be indicated through X-rays. The thyroid and kidney function tests would determine how the hormones are being produced and used in the body. MRI technique can be used to find out if the pituitary has suffered from any damage.
Treatment:
For previous some decades, doctors have been using synthetic growth hormones to treat growth hormone deficiency both in children and adults. When, before the mid-1980s, synthetic growth hormones were not available, doctors got natural hormones from cadavers and used them for this purpose. Injection of synthetic hormones involves some side effects, such as hip pain, curving of the spine, redness at the injection site and headache. As for as the duration of treatment is concerned, some people’s bodies start producing this hormone after some year of treatment, while others require the intake of synthetic growth hormone throughout their lives.
Diabetes Insipidus:
Do you know diabetes is not something strictly concerned with high blood sugar – it is a general term for a condition in which the body makes a lot of urine? Turning to diabetes insipidus, it makes you feel extra thirsty and, consequently, you keep on peeing a lot. Owing to insufficient production of antidiuretic hormone (ADH), the kidneys are unable to retain water and put out a lot of diluted urine. There are four different types of diabetes insipidus, namely, central diabetes insipidus (CDI), nephrogenic diabetes insipidus (NDI), dipsogenic diabetes insipidus (DDI), gestational diabetes insipidus (GDI). Caused by the damage to hypothalamus or pituitary gland, CDI is the most common type of DI. It results in the underproduction of ADH (Antidiuretic Hormone). When kidneys suffer from a damage and they are unable to respond to ADH, the condition is known as NDI. Malfunctioning of the thirst mechanism of the brain causes an individual to consume huge quantities of liquids, especially water. Such a condition is termed as DDI (dipsogenic diabetes insipidus). GDI occurs during pregnancy when mother’s own ADH is destroyed by an enzyme in the placenta.
Symptoms:
- Feeling of extreme thirst for water.
- Production of abnormally large quantity of pale or diluted urine.
- Delayed growth and dry skin.
- Bedwetting or unusually wet diapers.
- Loss of bodyweight.
- Irritability and muscle pains.
- Lethargy and unexplained weakness.
Diagnosis:
Excessive thirst and constant need for a bathroom serve as diagnostic sign for diabetes insipidus. Doctors take a series of blood or urine tests to confirm the presence of the disease. In order to check the response of kidneys to ADH, the doctors may give the victim an ADH substitute. Meanwhile, blood deprivation test may also be applied to check urine output, its composition, and blood sodium.
Treatment:
Each of the four types of diabetes insipidus requires a different type of treatment measure. The choice of a treatment method also depends on the severity of the condition. In case of minor issues of thirst and urination, the doctor may advise the victim to increase per day intake of water. The severe cases are to be treated through hormonal treatment and medications. Sometime, it is necessary to treat the underlying condition. The patients may also be asked to bring essential modifications in their diet and lifestyle.
Cushing’s Disease
Also known as Cushing’s syndrome, it is a disorder of the pituitary gland characterized by the abnormally high levels of the cortisol hormone. Owing to its association with the increased quantity of cortisol, it is also called hypercortisolism. One of the most common reasons for the onset of this disease is the overuse of corticosteroid medications. The unusually high levels of cortisol result in skin bruises, upper body weight gain and a round shaped face. Women may face menstrual irregularities and men may experience problems of erectile and infertility.
Symptoms:
- Abnormal weight gain.
- Deposit of fats in the facial region and between the upper back and shoulders.
- Appearance of stretch marks on the arms, abdomen and breasts.
- Thinning and bruising of skin.
- Slow healing of cuts, infection and insect bites.
- Fatigue and muscle weakness.
- Increased thirst and urination.
- Anxiety, depression and irritability.
Diagnosis:
Different types of blood and urine test have proved to be helpful in the accurate and timely diagnosis of this pituitary gland condition. The tests, like computed tomography (CT) scan, and magnetic resonance imaging (MRI) are used to determine the cause of excess cortisol production. Cushing’s syndrome is a rarely occurring hormonal disorder that affects adults between the ages 20 to 50.
Treatment:
The type of treatment measure to be suggested in this case depends on the underlying cause of Cushing syndrome. Certain medicines can be prescribed by your healthcare professional that can control cortisol production and ease the symptoms. The use of medication along with corticosteroids may require a change in the dosage. Surgery may be required for the removal of a cancerous or noncancerous tumor. Sometimes, chemotherapy and radiation are also recommended for the quick recovery of the patients.
Hypopituitarism
Referring to insufficient production of any of the nine hormones secreted by the pituitary gland, the term is modified as panhypopituitarism if deficiency occurs in most of the hormones. The accompanying symptoms may vary a great deal depending upon the deficiency of a particular hormone. Anyhow, the disease is confirmed through specific scans and blood tests, which can then be treated with the administration of deficient hormones by injection or tablets.
Symptoms:
- Excessive urination and thirst.
- Loss of appetite and stomach pain.
- Either weight gain or weight loss.
- Constipation, nausea and vomiting.
- Sensitivity to cold and stiffness in the joints.
- Decreased sex drive, infertility and loss of hair both in males and females.
- Headache and dizziness.
Diagnosis:
With the help of blood tests, a healthcare professional may come to know of the levels of the pituitary gland hormones in the body. The cause of the hypopituitarism can be determined by carrying out the MRI (Magnetic Resonance Imaging) of the pituitary gland. It will let you know about any damage or the development of a cancerous (malignant) or noncancerous (benign) tumor.
Treatment:
One of the ways to treat hypopituitarism is to orally intake the missing pituitary hormones and it may sometimes need to be continued for life. In case of sickness or being under stress, the individuals undergoing hormonal treatment may be asked to take an extra hormone, i.e. cortisone. If is a tumor (cancerous or noncancerous) is the culprit for hypopituitarism, it can possibly be treated with the help of radiation therapy or surgery.