What is Pancreas? Location And Diseases of Pancreas
What is Pancreas?
Some organs of the body serve as parts of more than one body systems. Pancreas gland is a good example of such body parts. Do you know what is Pancreas Function as the endocrine and exocrine organ?
Secreting more than a liter (around 1200 ml) of pancreatic juice daily, pancreas plays an important role in the digestive system. Shaped like tongue, the organ measures about 12 to 15 cm in length. In addition to working in the capacity of an exocrine gland, it also contributes to the endocrine system.

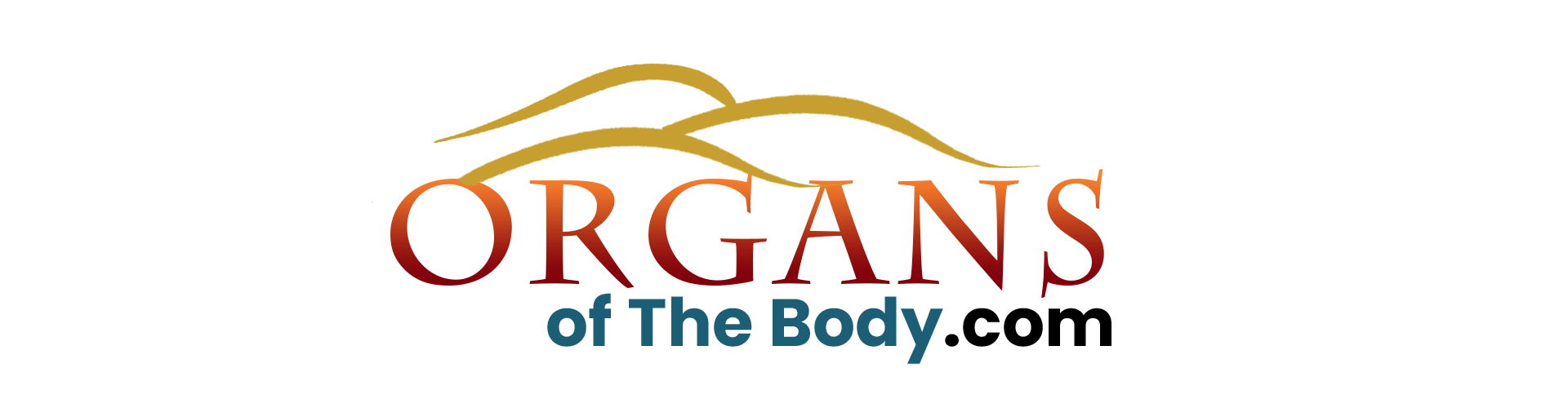
Fig. 1: Image of Pancreas
However, up to 80% to 85% of the organ is involved in exocrine function.
Table of Contents
Regarding pancreas role in digestion, it secretes enzymes which break down proteins, starch and fats. What are pancreatic enzymes names? Well, the pancreatic enzymes list includes trypsin, amylase and lipase, etc. On the other hand, as an endocrine organ, it produces insulin and glucagon.
Do you know the difference between endocrine and exocrine glands? A gland is an organ in your body that synthesizes and secretes substances like hormones and empties them either directly into the blood stream or into the cavities in the body.
The endocrine or ductless glands release secretions directly into the bloodstream. The circulatory system then carries and delivers these secretions to the target place. The exocrine glands, on the other hand, have ducts to carry their secretions to the target place. The uniqueness of pancreas lies in the fact that it works in both the capacities.
The pancreas diseases adversely affect pancreas and its functions in both digestive and endocrine systems. For example, in the absence of pancreatic juice, your small intestine won’t be able to digest proteins, lipids and carbohydrates in the semi-digested food coming from the small intestine.
Meanwhile, if the pancreatic juice does not contain enough insulin, it will lead to the condition called diabetes mellitus. The pancreas diabetes is characterized by the accumulation of sugar in the blood. However, an overworked liver and an unbalanced diet can also lead to the development of diabetes.
Pancreas Definition
After getting very basic and useful information about the organ, you must now be able to define it. The pancreas definition, as given in The Free Dictionary, is as under:
"Pancreas is a long, irregularly shaped gland that lies behind the stomach and secretes somatostatin, glucagon and insulin into the blood stream, and pancreatic juice containing pancreatic enzymes into the duodenum of small intestine."
Pancreas Location in Body
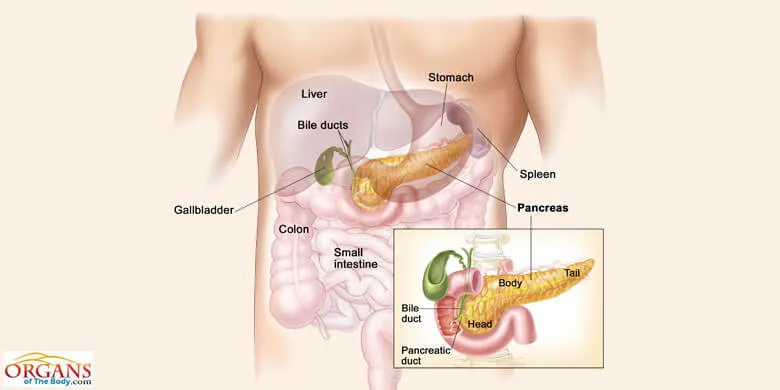
Fig. 2: Location of Pancreas in Human Body
You can find pancreas location in body in the vicinity of other abdominal organs, like liver, gallbladder, spleen, stomach and duodenum. Extending horizontally across the upper left abdomen, it is located behind the stomach. Duodenum, the first portion of the small intestine, forms a loop to nestle the pancreas.
As you can see in the pancreas diagram and pictures showing other organs as well, it extends to the spleen on the left side and is nestled between the kidneys. At the same time, the duodenum can be seen looping around it.
What is the pancreas color? While in the normal healthy condition, it looks pinkish-yellow. Concerning dimensions, it can be 6 to 8 inches long, 1.5 inches wide and 1 inch thick.
Pancreas Anatomy
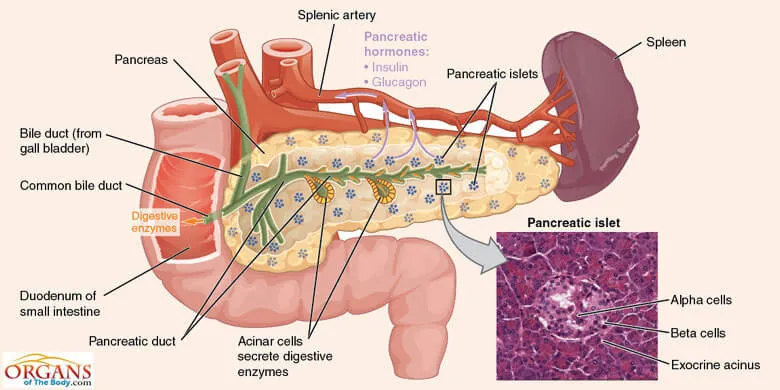
Fig. 3: Pancreas Anatomy
Shaped like a flat pear or fish, the pancreas is easily distinguishable into four major parts, namely, the head, the neck, the body and the tail. Looking deeper into the pancreas anatomy, you will come across the small endocrine portion and the large exocrine portion. Each component has its own unique anatomy and the functions to perform.
The characteristic feature of the pancreas, the endocrine cells are aggregated into small masses to form the pancreas islets of Langerhans.
The exocrine component of the organ is composed of the pancreatic acinar cells which are arranged in spherical masses, called acini. The acini, in turn, are grouped to form lobules. Other components of the pancreas include ducts, vessels, nerves and the connective tissue.
The head of the pancreas is its wide part positioned towards and nestled by the loop formed by the first part of small intestine. It is located at the juncture between stomach and duodenum. This is where the pancreatic juice is emptied into the intestine as partially digested food is released by the stomach.
Then comes the neck which joins the head with the body. And the body is the main part of the organ. At the end of the body, there is a thin tail which extends to the left.
Pancreas Function
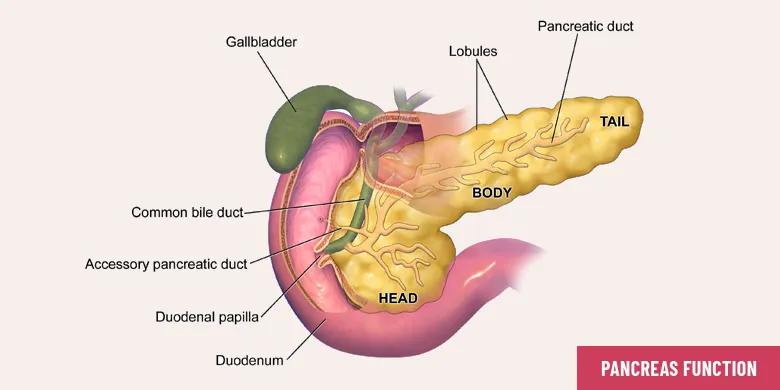
Fig. 4: Functions of Pancreas in Human Body
Pancreas function in human body is of incredible importance. Both pancreas and liver strive to regulate homeostasis and substances in the body. The pancreas performs several jobs of both the endocrine and exocrine nature.
The major part of the organ is composed of the exocrine tissue. Researchers at the Pancreas Center, Columbia University, suggest that about 95% of the organ consists of exocrine tissue that synthesizes several pancreatic enzymes to aid in digestion.
The remaining 5% of the pancreas is composed of endocrine cells, called the pancreas islets of Langerhans. Appearing like bunches of grapes, these clusters of cells produce pancreas hormones to regulate both the blood sugar level and the pancreatic secretions.
Secretion of the correct chemical substance in the proper amounts at the right times serves as an indication of the good pancreas health.
Pancreas Endocrine Function
Though making up just 5% of the organ, the endocrine tissue or the islets of Langerhans perform some important endocrine functions through the hormonal secretions. The islet hormones are produced by five different types of cells. Each cell type has its own unique secretary granule morphology, specific endocrine, paracrine and neuronal interactions, and different peptide hormone content.
Pancreas as an endocrine gland secretes some very useful hormones including insulin, glucagon, somatostatin, pancreatic polypeptide and ghrelin.
Let’s have an overview of the pancreas hormones with the sites of their secretion and associated functions:
Insulin: Banting and Best, in early 1920s, identified insulin secreted by endocrine pancreas as an antidiabetic hormone – a milestone in the understanding and treatment of diabetes mellitus. This hormone plays the primary role in maintaining the glucose homeostasis.
The extracellular glucose concentration is largely responsible for controlling the rate of insulin biosynthesis. Low basal rate of synthesis of pancreas insulin is maintained at the normal fasting glucose concentrations in the blood.
On the other hand, an increase in the blood glucose above the fasting level triggers a dramatic increase in the rate of insulin synthesis.
Glucagon: An important pancreatic hormone, glucagon plays a critical role in regulating glucose homeostasis. This peptide hormone performs functions that contrast with that of insulin. The former increases the level of blood sugar while the latter lowers the elevated level of blood sugar.
Responding to the abnormally low contents of sugar, glucagon is released that stimulates the cells in liver for the conversion of glycogen into glucose which is then poured into the bloodstream.
Low blood glucose level triggers the secretion of glucagon both directly and indirectly with the help of central and autonomic nervous system. Meanwhile, the “switch-off” signal of insulin/zinc ion also stimulates the secretion of glucagon.
On the other hand, the secretion of insulin and zinc ions by the beta cells serves to suppress the glucagon synthesis. High glucose level and somatostatin hormone also play a role in suppressing the glucagon secretion.
In both Type 1 and Type 2 diabetes, the levels of circulating glucagon are often elevated leading to glucose toxicity and exacerbation of the diabetic disorder.
Somatostatin: Somatostatin is an inhibitory hormone that suppresses the secretion of both insulin and glucagon hormone in a paracrine manner. It is largely through the interstitial communication between alpha and delta cells that somatostatin exerts its suppressive effect on glucagon secretion.
Secreted by delta cells of pancreas, this peptide hormone is transported to various parts of the body for performing its prohibiting and regulatory role in the endocrine system.
High glucose has suppressive effect on the glucagon secretion. But in case of somatostatin, it plays the reverse role, stimulating the production of this hormone.
Pancreatic Polypeptide: The PP cells of the endocrine pancreas are responsible for the secretion of pancreatic polypeptide hormone. Pancreatic polypeptide is abbreviated as PP. According to Mulholland et al. (2012), the physiological role of the 36-amino-acid pancreatic polypeptide remains unclear. However, this hormone plays inhibitory role in the pancreatic exocrine secretions and gallbladder emptying.
The cholinergic innervation is said to play predominant role in regulating PP secretion. Diabetes and normal aging bring an increase in PP secretion and the circulating PP level rise.
Pancreas Exocrine Function
In this type of pancreas function, the secretions are not released into the bloodstream, but are transported to the duodenum of small intestine via a tube called pancreatic duct. The pancreatic juice contains a number of valuable substances (e.g. digestive enzymes) that facilitate the functions of your gastrointestinal system, especially the breakdown of dietary contents, viz. fats, saccharides, and proteins. Some of the most important pancreas exocrine functions are summarized as under:
Neutralization: The partially digested food mass (chyme) that enters the duodenum through pyloric sphincter is highly acidic in nature. It needs to be neutralized for the proper action of intestinal enzymes.
The pancreatic juice has a large concentration of bicarbonate ions which make it highly alkaline in nature. This alkaline juice has the potential to neutralize the acidity of the chyme in the intestine. In addition to providing suitable pH for optimum enzyme action, the neutralization action of the pancreas also helps protect the wall of intestine from the destructive action of acid in the chyme.
Pancreas as Digestive Gland: Pancreas as digestive gland secretes over a dozen digestive enzymes which are specialized to act on various food components, like carbohydrates, proteins and lipids. (Sembulingam et al., 2012)
Enzymes in the pancreatic juice include trypsin, chymotrypsin, carboxypeptidases, nucleases, elastase, collagenase, pancreatic lipase, cholesterol ester hydrolase, phospholipase A, phospholipase B, colipase, bile-salt-activated lipase and pancreatic amylase.
Trypsin and chymotrypsin act on proteins to give polypeptides as end products. The job of pancreatic amylase is to break down starch into dextrin and maltose. Pancreatic lipase, on the other hands, splits triglycerides into monoglycerides and fatty acids.
The products of digestion are directly absorbed into the bloodstream across the intestinal wall and are transported to every cell in the body. A mitochondrion in the cell extracts energy from the food molecules in the form of ATP (Adenosine Tri-Phosphate).
Regulation of Pancreatic Secretions
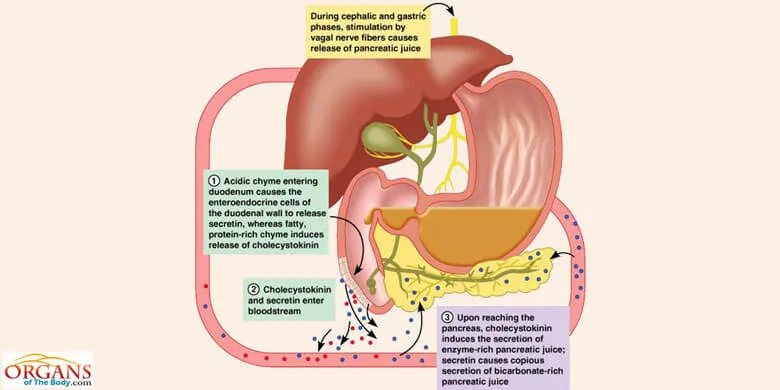
Fig. 5: Regulation of Pancreatic Secretions
If there is no mechanism for regulating the pancreatic secretions, it will produce either insufficient or undesirably high quantities of enzymes, hormones and other substances. And it will be difficult for your body to cope with such insufficiencies or excesses.
Your body has a sophisticated mechanism to regulate the secretion of pancreas in the body. It involves both nervous and hormonal factors which initiate and control each stage of pancreatic secretions.
Just like the gastric juice, the pancreatic juice is secreted in three stages which are the cephalic, gastric and intestinal phases. A nervous mechanism regulates the cephalic phase through unconditioned or the inborn reflex and conditioned reflex. The reflex response acquired by previous experience is called conditioned reflex.
The gastric phase of pancreatic secretion starts as food enters the stomach. The gastrin hormone controls the gastric phase. After its secretion in the stomach, the gastrin hormone is transported to pancreas through blood to stimulate the pancreatic secretion. The pancreatic juice, thus produced, has a high concentration of enzymes.
The chyme entering the small intestine from stomach triggers the intestinal phase which is under hormonal control. Some of the hormones stimulate the pancreatic secretion while others play an inhibitory role. The action of secretin leads to the secretion of pancreatic juice rich in bicarbonate ions. Cholecystokinin, on the other hand, makes the juice rich in enzymes.
The S cells of mucus membrane in duodenum and jejunum produce secretin while cholecystokinin is secreted by I cells in duodenal and jejunal mucosa.
Pancreas Facts
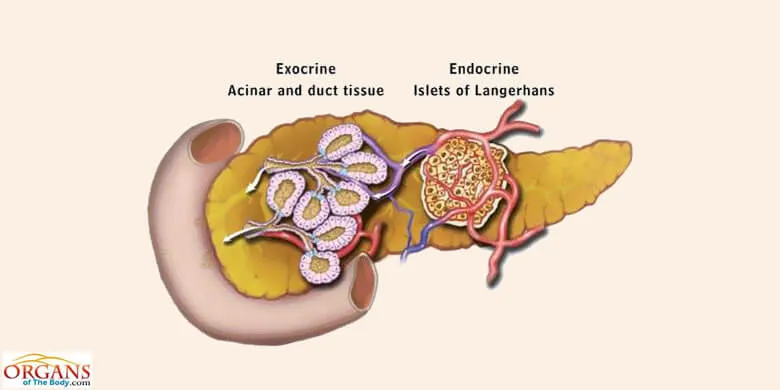
Fig. 6: Interesting Facts About Pancreas
The small, irregularly shaped gland, working in the capacity of endocrine as well as exocrine gland, was considered a hidden organ well into the twentieth century. Now, in 21st century, you know much about the pancreas anatomy and physiology. In other words, the pancreas is no more a pack of mysteries.
Let’s explore the pancreas structure and function from different angle and discover some really interesting pancreas facts.
- Serving in two capacities (endocrine and exocrine) at the same time does not affect the efficiency of pancreas. It works equally well in both the naturally assigned roles.
- Do you know even if the six salivary glands are removed from the mouth, the enzymes in the pancreatic juice can split all the starch from the food in the small intestine?
- If the gastric juice of the stomach cannot digest protein content of the food, the pancreatic juice is there to do the same job.
- The exocrine pancreas can produce as much as 1200 ml of pancreatic juice a day! The juice contains several digestive enzymes to split carbohydrates, proteins and fats.
- Owing to its mixed exocrine-endocrine function, the pancreas is also called a mixed gland.
- Do you know the endocrine component of the pancreas, forming just 5% of the organ receives five to tenfold higher pancreas blood supply than the larger (making up about 95% of the organ) exocrine compartment?
- The malfunctioning of the endocrine component of the pancreas results in the type 1 diabetes mellitus which accounts for 10% cases of diabetes in the world.
- Named after their discoverer Paul Langerhans, the islets of Langerhans comprise only 1 to 2 percent of the wet pancreas weight when the organ is fully grown up.
- There are approximately 1 million islets of Langerhans with uneven distribution throughout the pancreas.
- Usually leading to pancreas failure, the pancreatic cancer is one of the deadliest cancers and the fourth major cause of cancer-related deaths in the United States.
- The American Cancer Society predicted the deaths of around 31,800 individuals due to pancreatic cancer in 2005.
- In the year 2000, the World Health Organization (WHO) estimated an evidence of 213,500 deaths out of 216,400 cases of the pancreas cancer.
Pancreas Diseases
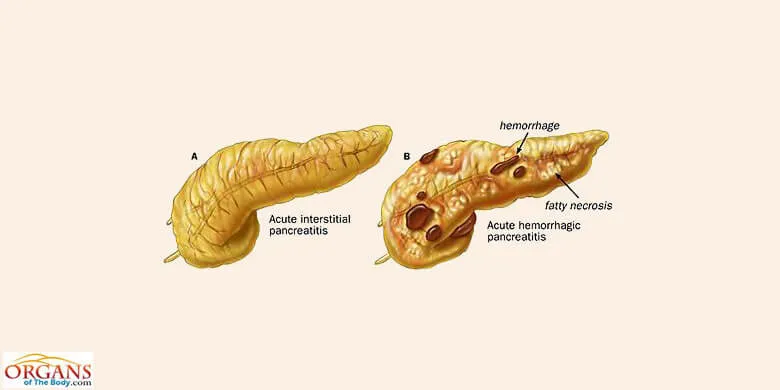
Fig. 7: Pancreas Diseases
Insufficient or excess secretions of pancreatic juice indicate pancreas problems. Some of the serious pancreas diseases include acute and chronic pancreatitis, pancreatic cancer and diabetes mellitus. Here follows a brief description of causes, diagnosis, symptoms, treatment and preventive measures for some of the pancreas diseases.
Pancreatitis
A rare but dangerous disease, pancreatitis is the inflammation of pancreatic acini. Forming the exocrine component of pancreas, acini are the spherical masses of the pancreatic acinar cells. The inflammation can be of two types, acute and chronic.
Though the acute condition subsides within days or a week, it may involve life-threatening complications, such as pancreas infection in the collected fluid, called pseudocyst. The chronic condition may cause permanent damage to the organ, resulting in pancreas failure. It can also cause diabetes mellitus.
Pancreatitis Causes
A more severe condition, acute pancreatitis occurs due to gallstones or the heavy intake of alcoholic beverages. On the other hand, the chronic pancreatitis occurs due to repeated attacks of acute inflammation or chronic damage to the organ.
Meanwhile, cystic fibrosis, malnutrition, congenital diseases of pancreatic duct, hereditary cause and long-time consumption of alcohol can also lead to chronic pancreatitis.
Diagnosis
Medical history, physical examination and blood tests are helpful in pancreatitis diagnosis. Your health care provider may also make use of ultrasound, pancreas x-ray, CT (Computed Tomography) and ERCP (Endoscopic Retrograde Cholangiopancreatogram) for the confirmation of acute and chronic cases.
Acute Pancreatitis Symptoms
According to Sembulingam et al. (2012), the commonly occurring acute pancreatitis symptoms include:
- Severe pain in the upper abdominal area.
- Fever and shock.
- Loss of appetite, followed by weight loss.
- Nausea, leading to vomiting.
Chronic Pancreatitis Symptoms:
- Constant or recurring abdominal pain in upper abdomen
- Pancreas back pain.
- Body weight loss.
- Bulky and floating stools.
- Swelling and tenderness of abdomen.
- Nausea, vomiting and fever.
Treatment
Acute swelling of pancreas requires immediate hospitalization and patients are not allowed to eat anything for several days. Stomach contents are emptied and drugs, like painkillers, pancreatic enzyme pills and antibiotics are given to relieve the symptoms. Pancreas surgery may be needed to remove gallstones.
The chronic pancreatitis occasionally requires the complete or partial pancreas removal through surgical operation.
Prevention
You can minimize the chances of the attack of pancreatitis by taking healthy diet and avoiding excessive consumption of alcohol.
Pancreatic Cancer
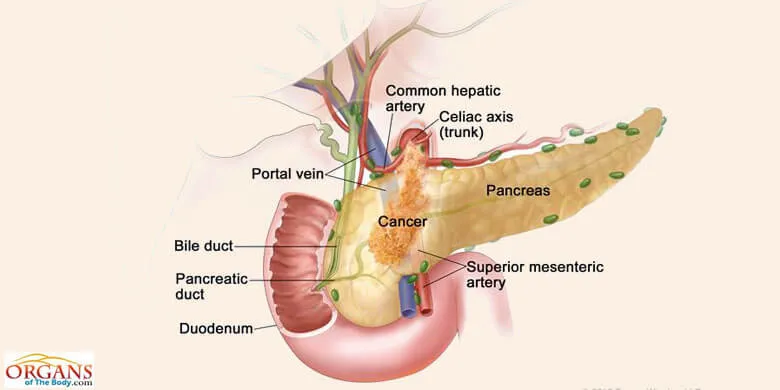
Fig. 8: Pancreatic Cancer
Despite significant scientific advances in the past five decades, the pancreas cancer remains one of the deadliest cancers in the US. The 5-year survival rate for this condition is even less than 5 percent. In the United States, the fourth major cause of cancer-related deaths is the pancreatic adenocarcinoma.
Pancreatic cancer refers to the growth of malignant cells in the pear-shaped organ located just below and behind the stomach, the pancreas. As it grows, the malignancy may block the bile duct and impair the process of digestion in the small intestine.
Margolis (2004) talks about the causes, diagnosis, symptoms, treatment and preventive measures for pancreatic cancer as given below.
Causes
Though the exact causes are unknown, pancreatic cancer is 2 to 3 times more common in heavy smokers than those who don’t smoke. Other possible pancreatic cancer causes include hereditary pancreatitis and exposure to solvents, petroleum and compounds of coal tar.
Diagnosis
It is extremely difficult to diagnose pancreatic cancer in early stages. Usually, the cancer has progressed to dangerous stages by the time the symptoms start appearing.
For diagnosis, initially abdominal and chest x-rays are performed. However, 80 percent of the cases are detected by pancreas ultrasound and CT scans. Pancreas biopsy is used to confirm the disease.
Pancreas Cancer Symptoms
Usually appearing at the later stages, the pancreatic cancer symptoms include:
- Poor appetite and weight loss.
- Severe pain in the right or upper central abdomen which may spread to the back. It may disappear by sitting up and leaning forward.
- Nausea, vomiting, feeling of fullness and itching skin.
- Jaundice.
- Pale stools or dark colored urine.
- Constipation or diarrhea.
- Fatigue and mood swings.
- Chills, dizziness and muscle spasms.
Pancreas Cancer Treatment
If the cancerous pancreas tumor is small and has not spread to other parts, it can be removed surgically. Sometimes, surgery for pancreas tumor treatment involves the removal of the entire organ along with a portion of the small intestine.
Radiation therapy in combination with chemotherapy can be used to destroy the cancerous cells and relieve the symptoms. For relieving pain, doctors may recommend the use of narcotics and analgesics. Pancreatic enzyme pills are used in case of the poor absorption of food owning to the blockage of pancreatic secretions.
Prevention
For pancreatic cancer prevention, you should minimize exposure to toxic, carcinogenic substances at home and in the workplace. Avoiding the use of cigarettes is also essential.
References
- Stewart, R. S., & Langford, K. (2015). The Everything Guide to Anatomy and Physiology: All You Need to Know about How the Human Body Works. " F+ W Media, Inc."
- Brant, W. E., & Helms, C. A. (Eds.). (2012). Fundamentals of diagnostic radiology. Lippincott Williams & Wilkins.
- Beger, H. G., Buchler, M., Kozarek, R., Lerch, M., Neoptolemos, J. P., Warshaw, A., ... & Shiratori, K. (Eds.). (2009). The pancreas: an integrated textbook of basic science, medicine, and surgery. John Wiley & Sons.
- Zachary, J. F., & McGavin, M. D. (2016). Pathologic Basis of Veterinary Disease Expert Consult-E-BOOK. Elsevier Health Sciences.
- Lee, C. (2004). Understanding the body organs & the eight laws of health. Brushton, N.Y: TEACH Services.
- Pancreas. (2017, June 29). Retrieved from https://www.thefreedictionary.com/pancreas
- The Pancreas and Its Functions. (2017, June 29). Retrieved from https://columbiasurgery.org/pancreas/pancreas-and-its-functions
- Chiras, D. (2013). Human Body Systems: Structure, Function, and Environment. Burlington, MA: Jones & Bartlett Learning.
- Norton, J., Bollinger, R. R., Chang, A. E., & Lowry, S. F. (Eds.). (2012). Surgery: basic science and clinical evidence. Springer.
- Islam, M. (2010). The islets of Langerhans. Dordrecht London: Springer.
- Montague, W. (1983). Diabetes and the endocrine pancreas: a biochemical approach. London: Croom Helm.
- Mulholland, M. W., Lillemoe, K. D., Doherty, G. M., Maier, R. V., Simeone, D. M., & Upchurch, G. R. (2012). Greenfield's Surgery: Scientific Principles & Practice. Lippincott Williams & Wilkins.
- Sembulingam, K., & Sembulingam, P. (2012). Essentials of medical physiology. JP Medical Ltd.
- Eroschenko, V. & Fiore, M. (2008). DiFiore's atlas of histology with functional correlations. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins
- Beger, H. G., Matsuno, S., & Cameron, J. L. (Eds.). (2008). Diseases of the pancreas: current surgical therapy. Springer Science & Business Media.
- Margolis, S. (2004). The Johns Hopkins complete home guide to symptoms & remedies: the complete reference to more than 500 symptoms & conditions. New York: Black Dog & Leventhal Distributed by workman Pub. Co.